By Dr. Colin Michie FRCPCH
The most likely benign tumour to develop in young women is a uterine fibroid. These grow in over a third of women by 35, and two thirds by 50 years of age. Most fibroids do not cause symptoms. However, between a quarter and half will need treatment. They can be troublesome, causing pelvic pain, infertility, excessive menstrual bleeding, urinary problems and constipation. So although biologically benign, they can profoundly affect a young woman’s quality of life, sometimes contributing to social isolation and related mental health challenges.
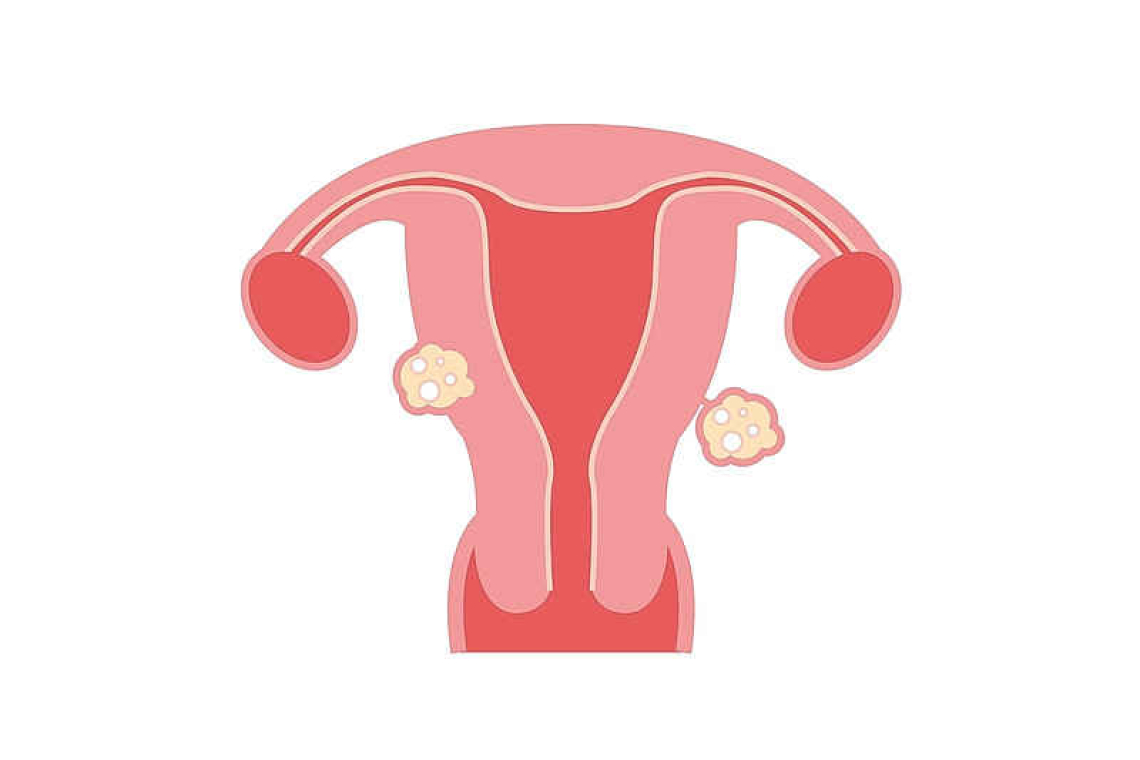
Benign tumours occur in all of us. Although they are referred to as benign, they can cause problems. They usually grow larger, but do not spread like malignant tumours. For instance, benign tumours like lipomas (from fatty tissues), or naevi (‘moles’) often make lumps on the skin. Adenomas of the colon, liver or glands are found unexpectedly on many scans, but do not usually need treatments. Meningiomas and gliomas are benign tumours of the brain or spinal cord. These sometimes cause concern because as they grow they may compress and compromise the nerves or the brain. Fibroids probably originate from stem cells in the muscular tissues of the uterus in women of reproductive age. They vary in size and number. Black women suffer more, often from an earlier age, too, with larger fibroids. Women with a higher BMI are also more likely to develop them. Fibroids usually (but not always) regress after the menopause.
Also known as leiomyomas, fibroids grow in the lining of the uterus, in the muscle itself, or next to the cavity of the uterus. Their growth is driven by the sex hormones oestrogen and progesterone, along with abnormal signal systems inside their cells. Ways to silence these systems are being tested. Fibroids less than two centimetres in diameter are unlikely to cause problems. Those five centimetres or greater in diameter are likely to stretch the uterus and compress nearby pelvic organs – the gut and bladder. These changes cause cramping pains, as does degeneration within the fibroid itself. Depending on their position, most larger fibroids are likely to increase a woman’s blood loss during periods and are more likely to reduce the chances of her conceiving.
Blood loss from fibroids often leads to anaemia if the number of red cells in the circulation falls. This slow and subtle problem can have many effects. Anaemia damages intellectual performance and memory; it causes fatigue, heart palpitations, restless legs, poor sleep, anxiety and possibly food cravings for unusual substances such as ice or clay. In many parts of the Caribbean, it is difficult to make up for iron loss with just a good diet, because iron is difficult to absorb. Common parts of a normal diet, including coffee, teas, oats, some cassava, soya or eggs are likely to bind to most of the iron in the gut. This means the body does not absorb it. So a prescription for iron by mouth, or possibly injection, may be required to make patients feel better.
Medications for fibroids should limit fibroid growth and control pain. Therapies with oral contraceptives, nonsteroidal anti-inflammatory drugs and hormonal therapies may succeed by reducing oestrogen. Vitamin D and green tea are recommended, too – both are effective treatments. Compounds that block progesterone receptors such as ulipristal acetate offer advantages to some women. These strategies reduce fibroid size and are often used before surgery.
Operations are directed at reducing fibroid size, while preserving a woman’s fertility. Local surgery or myomectomy within the uterus are a first stage. Blocking a fibroid’s blood supply, or killing their cells using high-intensity focused ultrasound, or heat from radiofrequency devices may be recommended. Removal of the uterus (hysterectomy) is a final option. Artificial intelligence systems, improved imaging and some robotic devices are being used by some surgeons to improve diagnoses and surgical methods.
Fibroids can develop alongside less common other uterine problems. These include endometriosis, polycystic ovarian syndrome and sometimes early malignancies of the cervix, uterus or ovaries. All can start with similar symptoms. So if you are concerned, a thorough check-up is both crucial and reassuring! Ultrasound scans can provide accurate three-dimensional views of the uterus, along with any fibroids and their blood supply. These help a gynaecologist make a sound diagnosis.
Women face challenges in their health care. Studies of fibroids in different societies have identified a lack of knowledge about these and other common women problems. Developing new treatments is slow because research into these unmet needs is poorly funded. In March 2024, an executive order in the US directed an innovative federal commitment to tackle such issues politically. For smaller communities, caring attentively for women in all clinical services will improve the quality of life of those suffering with fibroids.
Useful resources: acog.org/womens-health/faqs/uterine-fibroids ~ nhsinform.scot/illnesses-and-conditions/nutritional/iron-deficiency-anaemia
Dr. Colin Michie specializes in paediatrics, nutrition, and immunology. Michie has worked in the UK, southern Africa and Gaza as a paediatrician and educator and was the associate Academic Dean for the American University of the Caribbean Medical School in Sint Maarten a few years ago.